Understanding the Type 2 Inflammation Connection
Helping your patients with allergic rhinitis, asthma, eczema, CRSwNP, EoE and food allergies get relief
SUPPORTED BY:

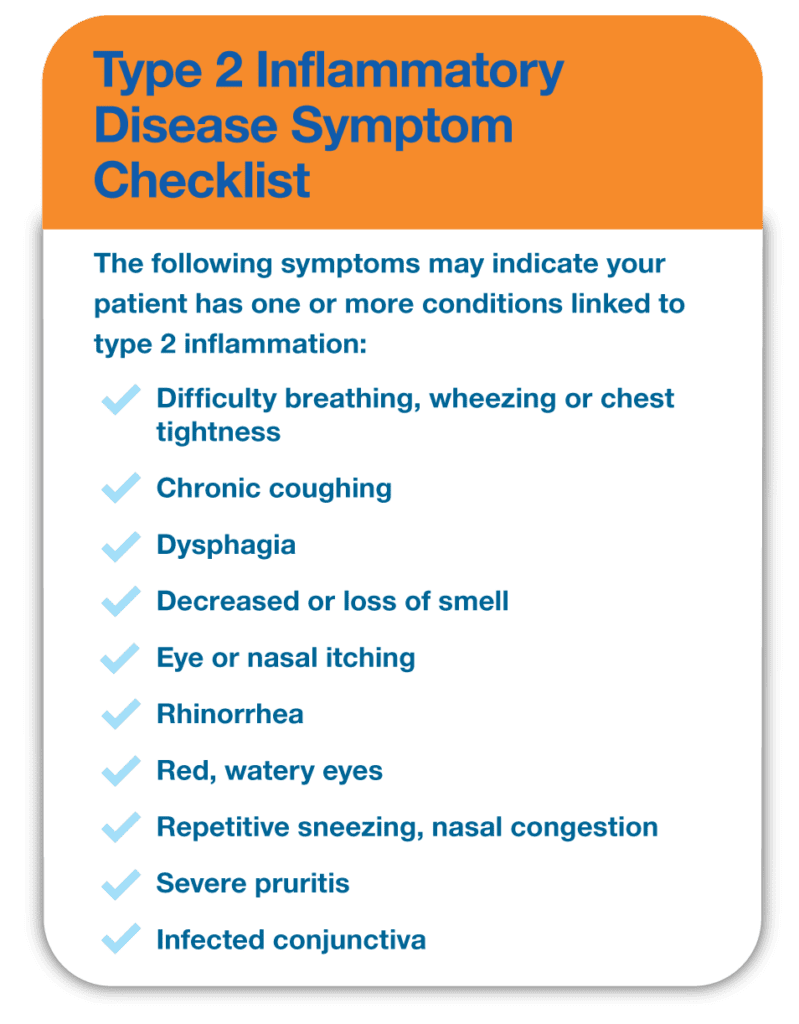
Rhinorrhea. Sneezing. Watery eyes. Chronic cough. Wheezing. Pruritis. Snoring. Dysphagia. Many of your patients may complain about these and other symptoms related to allergic rhinitis, asthma, atopic dermatitis (AD), chronic rhinosinusitis with nasal polyps (CRSwNP), eosinophilic esophagitis (EoE) or food allergies. In fact, some of your patients may suffer from symptoms associated with several of these conditions. That’s because they commonly occur together due to something called the allergic or atopic march – a progression of allergic diseases that may begin in early childhood as eczema and progress to other allergic conditions over time, including food allergies, hay fever and asthma. When this occurs, patients tend to suffer from more severe disease.
The common denominator? Type 2 inflammation due to an overactive immune response. The good news is that various treatments are available, including those that provide relief for more than one condition associated with type 2 inflammation. However, managing and treating these patients can be complex and may require specialized care. Board-certified allergists/immunologists specialize in diagnosing and treating type 2 inflammatory conditions and can partner with you and your patients to help them get relief. This site is designed to help you recognize conditions for which type 2 inflammation may be an underlying factor, understand how they are connected, and ensure your patients are diagnosed correctly and treated effectively.
Spectrum of Conditions
Hover Over the Icon Next to Each Condition to Learn More
Tap on the Icon Next to Each Condition to Learn More
- Nasal symptoms, including congestion, rhinorrhea or postnasal drip, repetitive sneezing
- Nasal, throat, eye itching
- Red, puffy watery eyes
- Nasal symptoms, including congestion, rhinorrhea or postnasal drip, repetitive sneezing
- Decreased or loss of sense of smell
- Snoring
- Feeding difficulties
- Failure to thrive
- Irritability
- Regurgitation/emesis
- Dysphagia
- Esophageal food bolus impaction
- Chest pain
- Frequent coughing and/or wheezing, especially nocturnal or exercise-induced
- Dyspnea
- Chest tightness
- Urticaria
- Angioedema
- Nausea, emesis, diarrhea
- Rhinorrhea
- Dyspnea
- Bronchospasm
- Dizziness
- Tachycardia
- Hypotension
- Shock
- Loss of consciousness
- Erythema or erythematous maculopapular rash
- Severe pruritis
- Dry skin, which can crack and bleed
The Conditions and Who’s at Risk
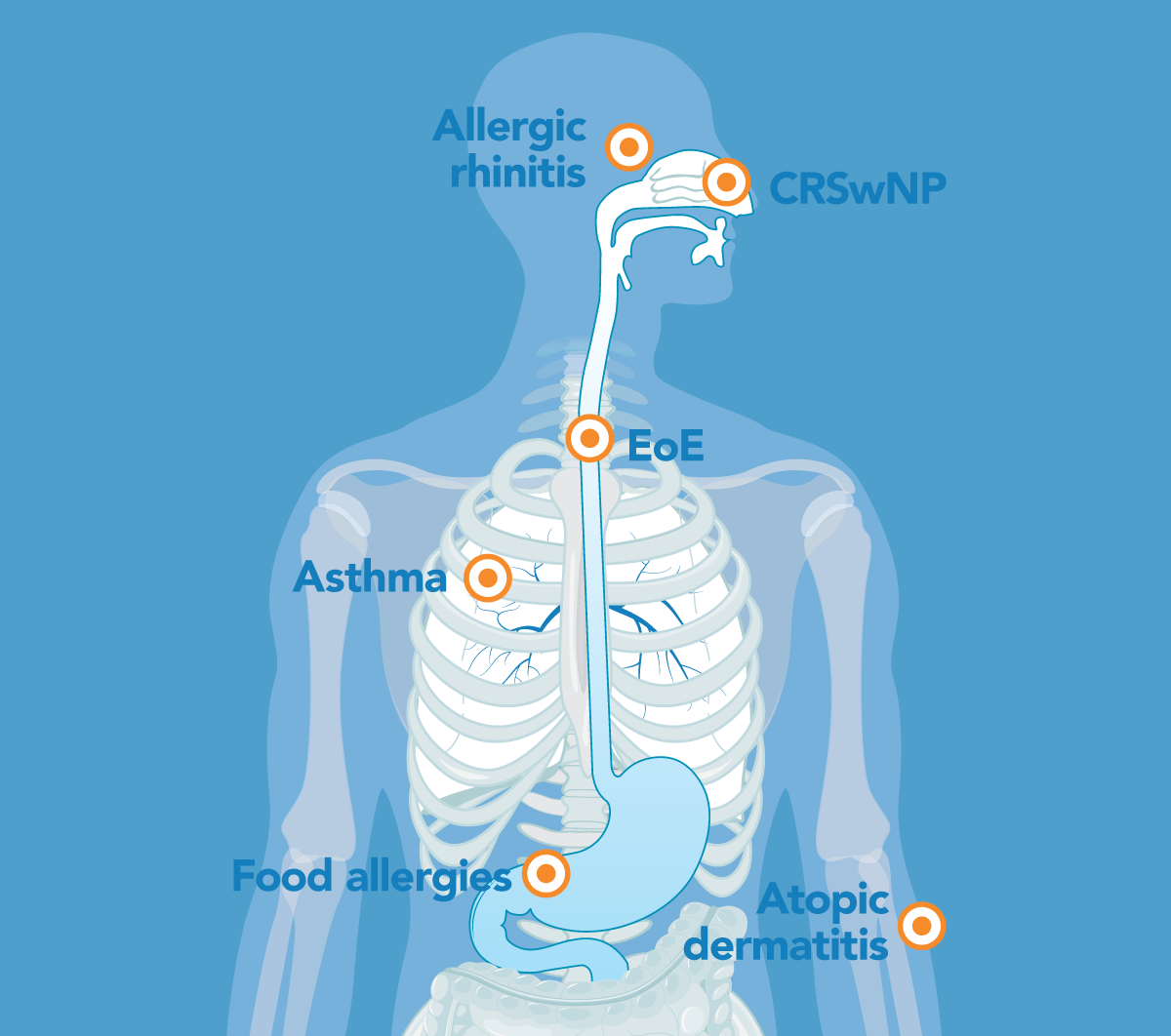
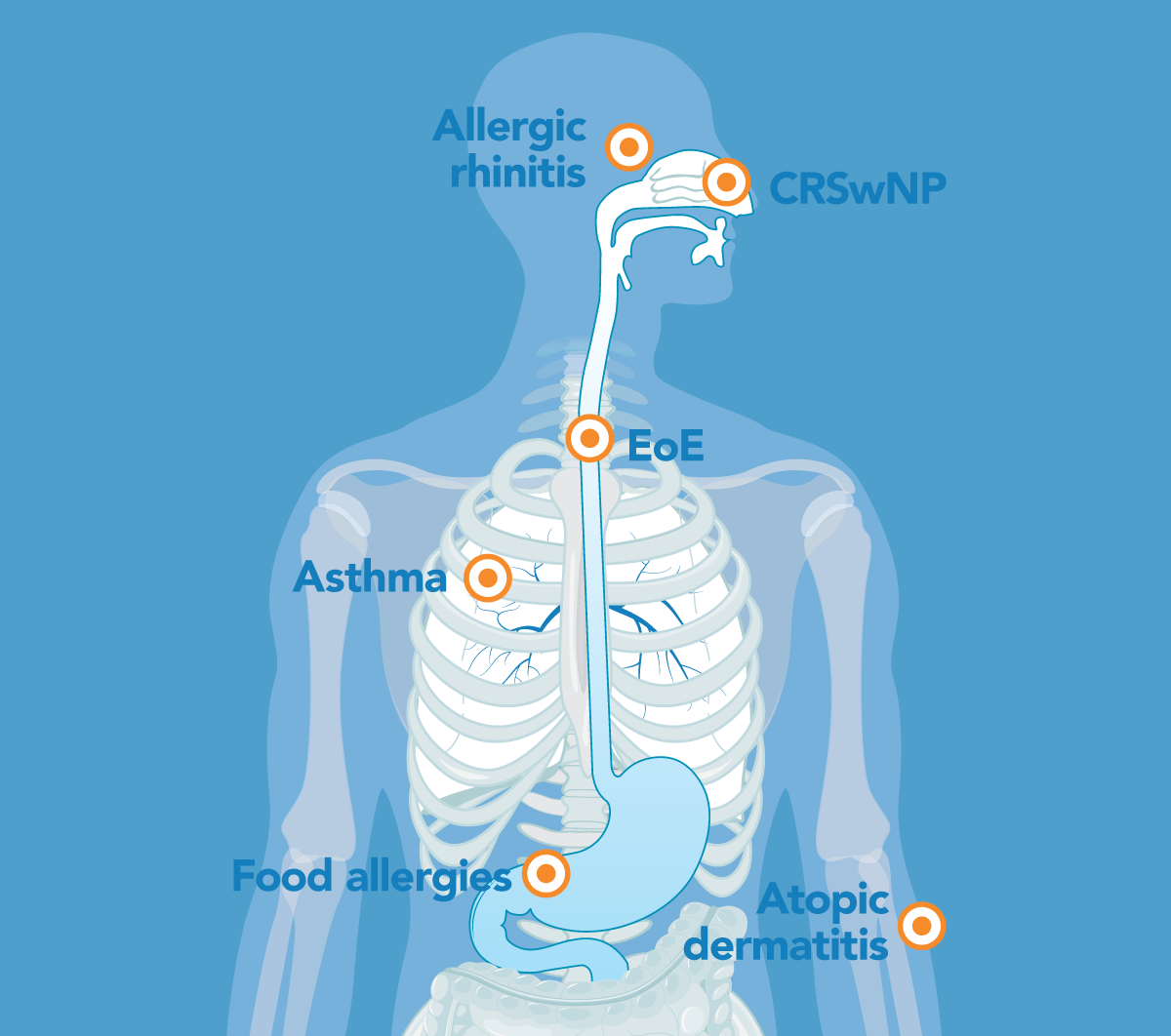
As a clinician, you know that the immune system is vital to survival but can sometimes overreact, leading to various health problems. Type 2 inflammation can be foundational to atopic and inflammatory diseases, resulting in an often overlapping spectrum of conditions and symptoms throughout the body, from the lungs and skin to the nasal passages, sinuses and esophagus.
The most common conditions for which type 2 inflammation may be an underlying factor are allergic rhinitis, asthma, AD, CRSwNP, EoE and food allergies. Many people have more than one condition associated with type 2 inflammation, and some have several. Board-certified allergists/immunologists can assess if type 2 inflammation is playing a role in the disease and determine appropriate treatment.
Hover over each condition to learn more.
Allergic rhinitis
Asthma

Atopic dermatitis (AD)
Chronic rhinosinusitis with nasal polyps (CRSwNP)
Eosinophilic esophagitis (EoE)
Food allergies
Allergic rhinitis, sometimes called hay fever, is a common condition affecting 15% to 30% of Americans. Allergens ranging from pollen and animal dander to dust mites and others can cause an allergic reaction seasonally or year-round with symptoms including rhinorrhea, repetitive sneezing, nasal congestion, postnasal drip and nasal, throat and eye itching.
- Up to 40% of patients with allergic rhinitis have asthma
- 17.4% of patients with allergic rhinitis have AD
Learn more about allergic rhinitis.
Asthma is a chronic disease that inflames and narrows the airways in the lungs. Patients may complain of coughing, dyspnea, chest congestion, tightness and wheezing. Each patient’s experience with asthma is unique and can range from mild to severe and even be life-threatening.
- About 24% of adults with moderate-to-severe asthma have more than one disease for which type 2 inflammation is an underlying factor
- An estimated 40% to 60% of people with severe eosinophilic asthma have CRSwNP
Learn more about asthma.
AD, also called eczema, develops in one out of 10 people during their lifetime. It affects up to 25% of children and 2% to 3% of adults. AD causes severe, persistent pruritus and moderate-to-severe erythema or erythematous maculopapular rash and excoriation. It can come and go over time, resulting in very dry and sensitive skin and often is exacerbated by certain soaps, detergents and lotions.
- 46% of patients with moderate-to-severe AD have more than one type 2 condition and 16% have at least two
- About 31% of people with moderate-to-severe AD have asthma
Learn more about AD.
Chronic rhinosinusitis is a common condition of the paranasal sinuses, and about one in four people with the condition develop nasal polyps. CRSwNP can cause decreased or loss of smell, facial pressure, postnasal drip, upper teeth pain, snoring and frequent epistaxis.
- About 69% of people with moderate-to-severe CRSwNP have more than one type 2 condition and 36% have at least two
- About 50% of people with CRSwNP have asthma
Learn more about CRSwNP.
- About 75% of people with EoE have more than one type 2 condition
- Between 12% and 68% of people with EoE have asthma
Learn more about EoE.
Food allergy is a serious and potentially life-threatening medical condition. It affects about one in 10 adults and one in 13 children. The majority of reactions are caused by eggs, cow’s milk, peanuts, tree nuts, fish, shellfish, wheat, soy and sesame. Symptoms can range from mild (a few hives) to severe (anaphylaxis).
- 16% to 29% of children with food allergies have AD
- About 67% of people with EoE have food allergies
Learn more about food allergies.
Inflammation Cascade
Type 2 inflammation is the underlying factor for various allergic or atopic conditions, including allergic rhinitis, asthma, AD, CRSwNP, EoE and food allergies, which involve multiple organ systems.
Hover over the icons in the cascade below to learn more.
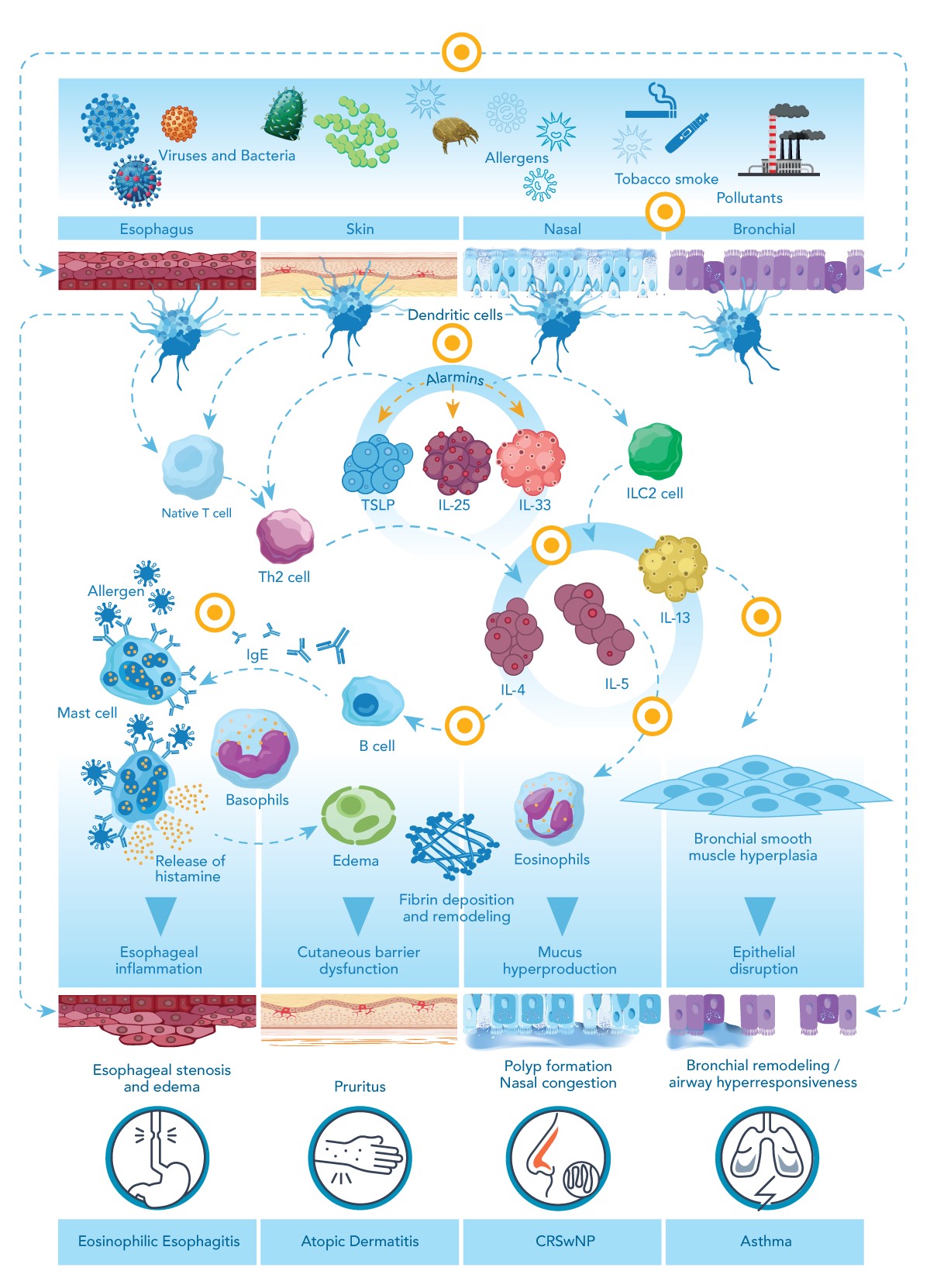
Note: This graphic is an oversimplification of the process, which features significant interaction between these pathways and involves other pathways that are not shown here, including independent sources of type 2 inflammation.
Diagnosis and Treatment
Diagnosing and treating allergic rhinitis, asthma, AD, CRSwNP, EoE and food allergies varies widely and may involve more than one specialist. A board-certified allergist/immunologist can diagnose and guide treatment of all these conditions, including determining whether they are associated with type 2 inflammation, which may influence the treatment plan. The allergist/immunologist will work with you and other specialists to address your patients’ underlying immunological inflammation.
Here’s how these conditions are diagnosed and treated.
Allergic rhinitis can make sufferers miserable. Most people manage it on their own or with your help using over-the-counter or prescription medications. When those don’t work, it may be time to refer your patients to a board-certified allergist/immunologist, who can work with you to guide their treatment.
The allergist/immunologist will take a detailed history to help reveal what might be causing the nasal and eye symptoms, including potential triggers in home and work environments. Other conditions, such as a deviated septum, can make allergic rhinitis more severe. In some cases, the allergist/immunologist may conduct an inhalant allergy test to determine the offending allergen.
Treatment:
Once the allergen is identified, it’s best to avoid it if possible or use methods to reduce it (e.g. closing windows when pollen counts are high). Depending on the allergen and patient, the allergist/immunologist might recommend:
- Intranasal corticosteroids
- Intranasal and oral antihistamines
- Oral and topical decongestants
- Leukotriene pathway inhibitors (which also are used to treat asthma)
- Eye allergy drops
- Subcutaneous or sublingual immunotherapy
Learn more about the diagnosis and treatment of allergic rhinitis.
There are many types of asthma including: allergic, non-allergic, adult-onset, occupational and exercise-induced bronchoconstriction. Each has its own triggers causing a variety of symptoms your patients need to manage. It’s time to refer them to a board-certified allergist/immunologist who can help you get their condition under control if their symptoms:
- interfere with normal activities,
- cause frequent coughing or wheezing – especially if it’s nocturnal or exercise-induced,
- require more than two corticosteroid bursts in a year,
- require use of quick-relief medication two or more times a week or
- result in an emergency department visit or hospitalization.
Diagnosis:
The allergist/immunologist can review the patient’s symptoms and family history, conduct lung function testing and screen for underlying type 2 airway inflammation. An allergy test and an in vitro blood test for allergens may also be part of the asthma workup to develop an individualized asthma action and treatment plan. Allergists/immunologists are trained to care for both adult and pediatric patients.
Treatment:
Effective treatment of asthma may include identifying and avoiding allergens that trigger symptoms of allergic asthma using drug therapies, minimizing the use of systemic corticosteroids and developing an emergency action plan for symptoms. Many of your patients with asthma will require one medication for quick-relief and another for long-term control; however, some medications can be used for both quick-relief and long-term control.
- Quick-relief rescue:
- Short-acting inhaled beta2-agonists
- Short-acting inhaled beta2-agonist with budesonide
- Short-acting anticholinergics
- Long-term control:
- Inhaled corticosteroids
- Long-acting inhaled beta2-agonists (LABA) with an inhaled corticosteroid
- Antileukotriene agents
- Long-acting anticholinergics
- Biologics
- Quick-relief rescue and long-term control:
- Formoterol (LABA) with an inhaled corticosteroid
For your patients whose asthma is triggered by an allergy, immunotherapy – either as subcutaneous injection or sublingual tablet – may be appropriate.
If your patient’s asthma is moderate to severe and uncontrolled, biologic therapies may be used to manage the condition and improve quality of life.
Learn more about the diagnosis and treatment of asthma.
You likely see and treat many patients with AD, but if a patient is developing severe pruritis, moderate-to-severe erythema, lichenification, excoriations or secondary infections, you should refer them to a board-certified allergist/immunologist who can work with you to treat them.
Diagnosis:
Since AD can be related to allergies, an allergist/immunologist can help your patients determine what exposure exacerbates the condition. They may conduct allergy testing to identify allergens and ask what soap, detergent or skin care products the patient uses that might make AD worse. An estimated one-third to two-thirds of young children who have moderate-to-severe AD have food allergies that an allergist/immunologist can also help manage.
Treatment:
Depending on the severity of the AD, an allergist/immunologist may recommend different treatments.
They may start by prescribing topical treatments, including:
- Corticosteroids
- Calcineurin inhibitor
- Phosphodiesterase inhibitor
- Topical JAK inhibitor
If those treatments don’t control the patient’s symptoms, the allergist/immunologist may prescribe a biologic, oral JAK inhibitor or other treatments
Learn more about the diagnosis and treatment of AD.
If a patient with CRSwNP has sleep disturbances and mouth breathing leading to poor work and school performance or decreased or loss of smell, a board-certified allergist/immunologist can help you evaluate their condition. Although CRSwNP is not cancerous, it can cause significant and frustrating symptomology. Anyone is at risk for CRSwNP, but it is more common in people with asthma and those who are 40 to 60 years old.
Diagnosis:
Nasal endoscopy is used to diagnose CRSwNP, and a CT scan may be necessary to confirm the diagnosis. If your patient’s CRSwNP is associated with type 2 inflammation, it may influence the treatment plan. The allergist/immunologist can help determine the underlying causes and may also work with an otolaryngologist during diagnosis and treatment.
Treatment:
Initial treatment to reduce nasal edema includes avoiding common triggers, such as tobacco smoke, aspirin or non-steroidal anti-inflammatory drugs (NSAIDs), chemical fumes, dust or debris, and incense. Home remedies include saline spray and rinsing out nasal passages with a Neti pot. If they don’t provide relief, the allergist/immunologist may prescribe a corticosteroid nasal spray or fluticasone breath-powered corticosteroid device. If the polyps are large and these medications aren’t beneficial, the otolaryngologist may recommend surgery to remove them and enlarge the sinus passages. Polyps often recur despite surgery and long-term treatment with nasal steroids may be necessary. Alternatively, the allergist/immunologist may recommend a biologic. Biologics have been shown to reduce the need for surgery and treatment with oral steroids.
Learn more about the diagnosis and treatment of CRSwNP.
Poor feeding, failure to thrive, food regurgitation, emesis or stomach pain in children, and dysphagia, food impactions or severe reflux in adult patients should prompt a referral to a board-certified allergist/immunologist who can collaborate with you and a gastroenterologist for testing and treatment.
Diagnosis:
An upper endoscopy will be performed by a gastroenterologist to confirm the diagnosis by conducting a biopsy of the tissue and checking for eosinophils. Once EoE is confirmed, the allergist/immunologist will assess your patient for potential food (the most common trigger of EoE) and environmental allergies.
- Topical steroids, e.g. budesonide oral suspension
- Proton pump inhibitors (PPIs)
- Diet elimination therapy of one or more of the most common foods known to trigger EoE (milk, eggs, wheat, soy, peanuts, tree nuts, and fish, including shellfish)
- Esophageal dilatation, which may be performed by the gastroenterologist if esophageal stricture is advanced
- Biologic therapy to reduce inflammation and improve symptoms
Learn more about the diagnosis and treatment of EoE.
Any patient who has had an immediate, severe allergic reaction to a food should be prescribed an epinephrine autoinjector and referred to a board-certified allergist/immunologist who can work with you in managing their condition. Food allergy symptoms are most common in babies and children but can appear at any age. Your patients may even develop an allergy to foods they have eaten for years with no problem. The most common food allergens are eggs, dairy, peanuts, tree nuts, fish, shellfish, wheat, soy and sesame. Symptoms can range from mild with just a few hives to anaphylaxis, which can be life-threatening.
Diagnosis:
An allergist/immunologist will obtain a detailed dietary history, including what food caused the reaction, how much they ate, how long it took for symptoms to develop, what symptoms they experienced and how long they lasted. The allergist/immunologist may conduct an allergy skin test and, in some cases, a blood test to measure the IgE antibody to the specific food tested. An oral food challenge may be conducted in the allergist/immunologist’s office if necessary to confirm the diagnosis and guide treatment.
Treatment:
Once a food or foods are identified as the culprit, the most important step is for your patient to avoid consuming that food. That includes closely reading labels for their food allergen. Patients with food allergens should also share information about their food allergy with servers when eating out at restaurants.
The allergist/immunologist will determine if the patient needs an epinephrine autoinjector and knows how and when to use it. While not a cure, some medications can reduce the risk of a severe allergic reaction by accidental ingestion. Biologics may address type 2 inflammation in adults and children one year of age and older with food allergy to help reduce allergic reactions and anaphylaxis that may occur with an accidental exposure to one or more foods. The allergist/immunologist may also discuss oral immunotherapy (OIT), a daily oral therapy that modifies the immune system.
Learn more about the diagnosis and treatment of food allergies.