Supported by:
![]()
Overview
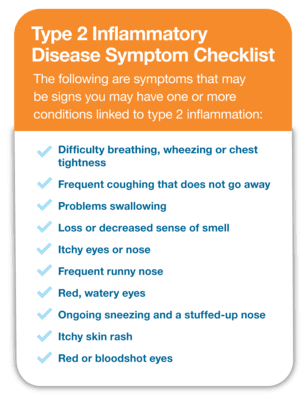
Frequent runny nose. Sneezing. Itchy skin, eyes or nose. Red, watery eyes. Wheezing. Coughing bouts. Problems swallowing. Recurring rashes, frequent swelling and itching. If you have one or more of these symptoms, you may have allergic rhinitis (hay fever), asthma, atopic dermatitis (eczema), chronic rhinosinusitis with nasal polyps (nasal polyps), eosinophilic esophagitis (EoE) or food allergies. These conditions often occur together, and having one places you at a higher risk of developing another, making you even more miserable. They can affect several areas throughout your body, from your nose, sinuses and lungs to your gastrointestinal tract, and even your skin.
In many cases, having one or more of these conditions is a sign that your immune system has an increased amount of type 2 inflammation. You may have had some signs earlier in your life that this was happening. Did you (or your child) have eczema as a baby, and then develop food allergies, hay fever or asthma? This is something called the allergic march, a progression in which one allergic condition can lead to the development of other allergic conditions over time as a result of increased type 2 inflammation.
The immune system is important for survival. It protects against infections and fights germs (bacteria, viruses and fungi) that can make you sick. However, in some people, the immune system overreacts because of genetic and environmental factors, resulting in excess type 2 inflammation. This overreactive type 2 immune response can cause inflammation that can harm certain organ systems in your body.
The good news is that various treatments are available, including those that can provide relief for more than one condition related to type 2 inflammation. If you suffer from conditions related to type 2 inflammation, it’s important to be evaluated by a board-certified allergist who specializes in diagnosing and treating type 2 inflammatory conditions and can work with your other health care providers to help you get relief.
Are you ready to take control of your allergies or asthma?
It’s time for an allergist.
Spectrum of Conditions
Hover over the icon next to each condition to learn more.
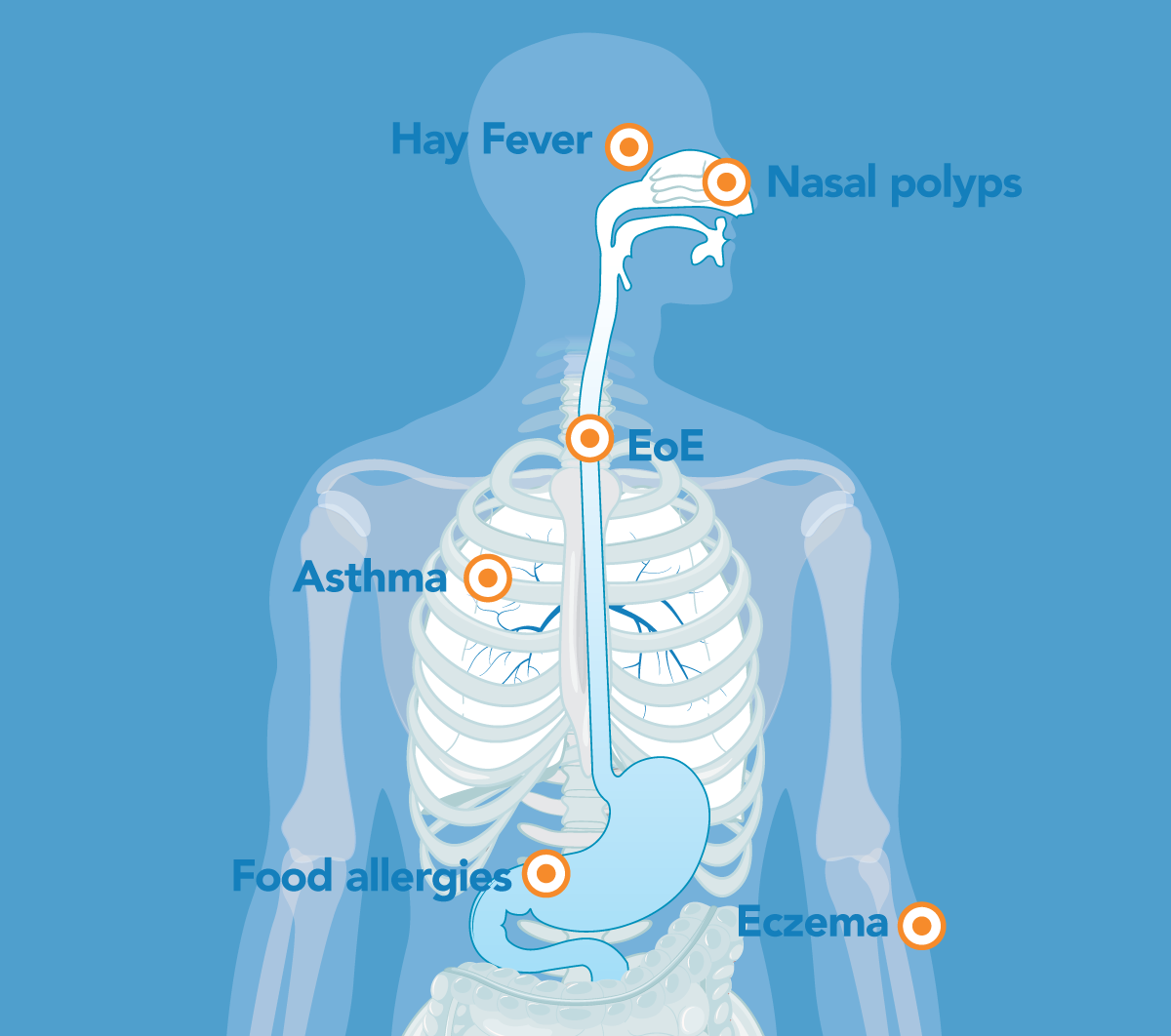
Some of the conditions that may be related to type 2 inflammation are:
- Allergic rhinitis (hay fever) – Allergic rhinitis – which is very common – is nasal inflammation caused by triggers such as pollen, pets, dust and other airborne substances. It can happen at certain times of the year (often spring or fall) or year-round and can make you miserable, causing everything from severe nasal congestion to a constantly runny nose to sneezing to an itchy nose, throat and eyes.
- Asthma – Asthma is a disease of the lungs that causes breathing problems in children and adults because of inflammation and narrowing of the lower airways in the lungs. You may cough, wheeze or have trouble breathing, and it can be life-threatening.
- Atopic dermatitis (eczema) – Atopic dermatitis is the result of an abnormal skin barrier causing excess skin inflammation. It is very common in children, and one in ten people will develop eczema during their lifetime. It can cause severe itching with dry, cracked, crusted and bleeding skin that can develop secondary bacterial infections if not treated. appropriately.
- Chronic rhinosinusitis with nasal polyps (nasal polyps) – About one in four people who have constant swelling and pain in their nasal passages (rhinosinusitis) develop nasal polyps, which are growths in the nose or sinuses. They are not cancerous, but they can cause loss of smell, facial pressure, postnasal drip, pain in your upper teeth, snoring and nosebleeds.
- Eosinophilic Esophagitis (EoE) – EoE causes inflammation and eventually narrowing and scarring of the esophagus (the tube that connects your mouth to your stomach). Infants and children may not be able to eat well. They may spit up, vomit or have stomach pain and might not grow like they should. Adolescents and adults with EoE often are the last ones to finish a meal and may complain of trouble swallowing or getting food caught in their throats.
- Food allergies – A food allergy is a serious and potentially life-threatening medical condition that is more common in children. The foods most commonly associated with food allergy in the U.S. are eggs, cow’s milk, peanuts, tree nuts, fish, shellfish, wheat, soy and sesame. Signs or symptoms of a food allergy can be an itchy rash (hives), swelling of the eyes or lips, vomiting, coughing or wheezing that typically occurs immediately – minutes – to hours after eating a trigger food. Most reactions occur within a few hours. The type of reaction you have can vary depending on a variety of factors and can be a few hives or a more serious allergic reaction called anaphylaxis. As a result, it is important for most individuals with food allergies to carry an epinephrine (adrenaline) autoinjector to address a severe allergic reaction in case they accidentally ingest food to which they are allergic.
Patient Journey to EoE
EoE is increasingly recognized as a major cause of swallowing difficulties in children and adults. Sometimes EoE can be mistaken for other conditions, such as gastroesophageal reflux disease (GERD). Learn more about how the journey to an EoE diagnosis can happen in children and adults.
The Type 2 Inflammation Connection
Having more than one condition related to type 2 inflammation is much more common than you may think. If you have one or more of these conditions, it may mean you have excess type 2 inflammation – but you don’t need to suffer. See an allergist to learn if you have a type 2 inflammatory condition and get relief.